understanding the importance of nerve protection
When surgeons embrace nerve protection as a part of their algorithm in the OR, they give their patients a better chance of functional recovery.
why nerves need protection after an injury
Because nerve damage can start from the inside out, an injury isn’t always obvious.
When a traumatic injury occurs, nerves near the site of impact may remain intact and appear outwardly normal. But damage often happens within the nerve or to the tissue surrounding it. Stretching and compressive forces of an injury can cause nerves to experience endoneurial and perineurial damage. In addition, a nerve that appears normal after trauma may become injured over time due to compression from the buildup of scar tissue in the environment surrounding the nerve.
- A deep dive into nerve protection:
- injury mechanism matters
- why protect
- when to protect
- the healing process
- promote healthy nerve anatomy
- solutions
Considerations for treating non-transected nerve injuries
The challenge here is the surrounding tissue, the scar bed, the zone of injury and how that’s going to impact recovery of the nerve.
— MEREDITH OSTERMAN, MD
injured nerves in continuity still need intervention
Despite complete nerve continuity preservation, stretching and compression injuries can result in permanent motor or sensory nerve deficits. While the nerve may not have been transected, they can lead to the same pain and loss of function if left untreated.1
77% of patients with hand/wrist trauma and subsequent nerve symptoms are not experiencing full nerve recovery (n=13).1
Understanding where and why non-transected nerve injuries present themselves, especially in acute hand and wrist trauma, can help in early intervention. And early intervention can help maximize functional recovery.
In the study “Nerves in Continuity Following Hand Trauma: A Descriptive Report,” certain mechanisms of injury and concomitant injuries had a higher likelihood of nerve involvement. For example, concomitant tendon and ligament injuries had a higher likelihood of nerve involvement (81.8% and 83.3%, respectively) compared to fractures (66.67%).1
- concomitant injury
- injury mechanism
percentage of patients with abnormal nerve symptoms by concomitant injury1
Tendon and ligament injuries were associated with an increased chance of nerve involvement (81.8% and 83.3%, respectively).1
percentage of patients with abnormal nerve symptoms by injury mechanism1
Blast injuries (such as from a firearm), crush injuries and compression injuries (such as from machinery) are strongly associated with nerve involvement.1
The study featured a retrospective cohort of 20 patients with hand or wrist trauma that presented at the initial surgery with intact nerves. Of these patients, 75% had signs of impaired nerve function either before surgery or at their first post-surgical follow-up. Only 23% experienced full sensory recovery and 57% had full recovery from pain without direct nerve treatment.1
study design: nerves in continuity following hand trauma
The study featured a retrospective cohort of 20 patients with hand or wrist trauma that presented at the initial surgery with intact nerves. Of these patients, 75% had signs of impaired nerve function either before surgery or at their first post-surgical follow-up. Only 23% experienced full sensory recovery and 57% had full recovery from pain without direct nerve treatment.1
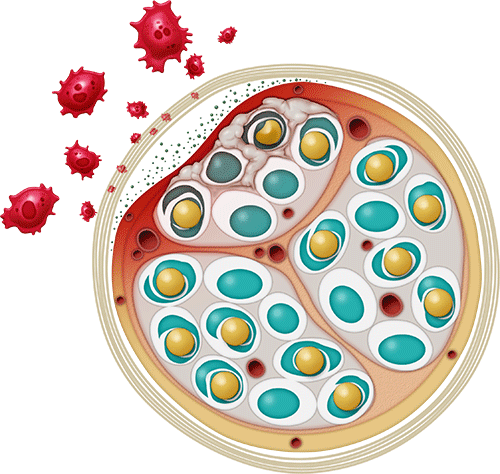
When a nerve is injured, it goes through a healing process in which inflammatory macrophages play a critical role in helping to repair the damaged tissue.
However, when there is ongoing irritation, such as a nerve rubbing against a plate or tethering due to scar tissue formation, that inflammation can become chronic and lead to additional scarring and pain.
Nerve protection preserves and protects nerves that may not have been cut or have obvious damage by helping to mitigate soft tissue attachment and block inflammatory macrophage invasion.2 Introducing a barrier between the non-transected nerve and its surrounding soft tissue creates a safer space for proper nerve regeneration.2
In one study of patients who presented with intact nerves at the time of surgery but experienced symptoms of nerve injury, only 23% experienced full recovery based on qualitative sensory assessments, in the absence of direct nerve treatment.1
what’s at risk when nerves aren’t protected
- Scarring
- Soft tissue attachment
- Compression
- Tethering
- Edema
- Reactive swelling
- Further injury
- Limited mobility
- Decreased sensation
- Incomplete recovery
how nerve protection helps
- Provides a protective barrier to separate the nerve from the surrounding tissues, minimizing the potential for soft tissue attachments to allow the nerve to glide2-4
- Reduces the likelihood of traumatized nerve becoming inflamed by serving as a barrier to inflammatory macrophages2
- Reduces the potential for nerve and neurostenalgia5
- Reduces the likelihood of collagen deposition (internal scarring) in the nerve2
Why prioritize nerve protection, even in non-transected nerve injuries?
If you don’t prioritize the nerve at the time of the injury, then you’re compromising the patient’s ultimate neurologic outcome.
— MICHAEL J. GARCIA, MD
Ensuring patients have the best possible chance for optimal recovery is always the goal. Because of this, protection should be top of mind whenever performing cases where a nerve is involved.
When it comes to nerves, don’t wait to see what transpires after acute surgical healing. Proactive protection sets patients up for long-term functional recovery.
Choosing candidates for nerve protection
When making decisions about candidates for nerve wrapping, the cases I consider are revision nerve releases, distal humerus fractures when they lie directly on the plate and crush injuries.
— SUNISHKA WIMALAWANSA, MD
nerve protection is beneficial for:
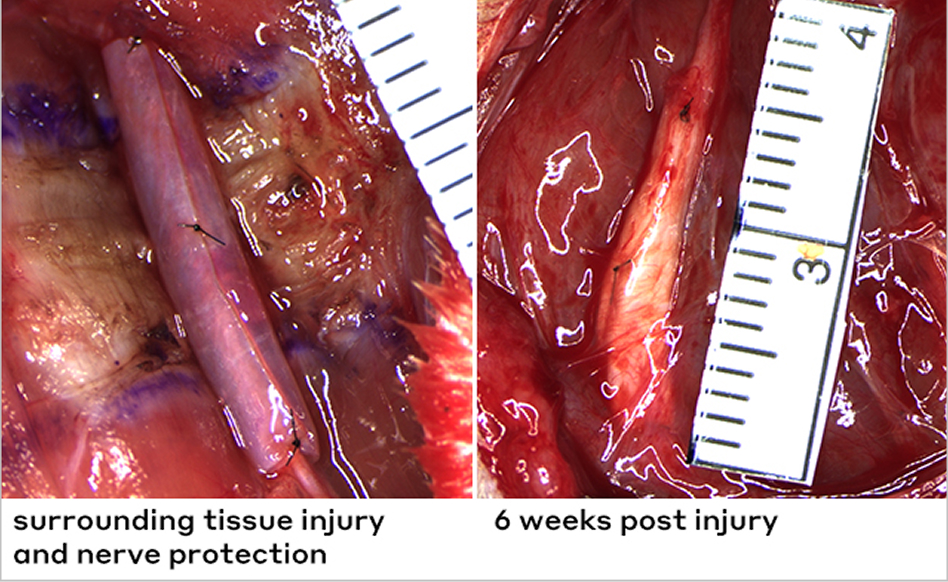
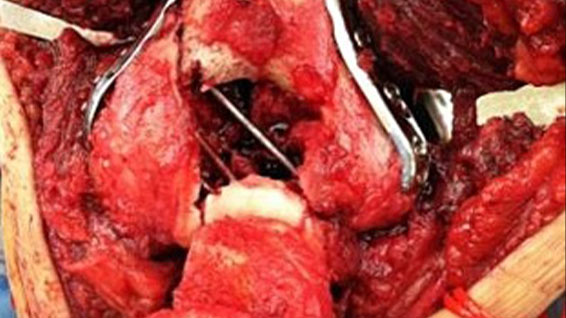 Photo courtesy of Peter Evans, MD, PhD
Photo courtesy of Peter Evans, MD, PhD
hardware-based procedures
Study results have clearly demonstrated the presence of marked inflammation and tissue reaction in the soft tissue covering stainless steel and titanium plates. This is shown to cause immune-inflammatory reactions.6 When near a plate, nerves can rub against the plate surface and incur mechanical irritation directly.

fractures
In one study, 67% of hand fractures presented alongside signs of associated nerve injuries (n=20).1 For humerus fractures, fracture location is an important indicator of the probability of a nerve issue. The radial nerve is most likely to be damaged when the middle portion of the bone is broken. The radial nerve is particularly vulnerable in this location because it is fixed and near the bone and cannot withstand the forces applied to it as a result of bone displacement.7
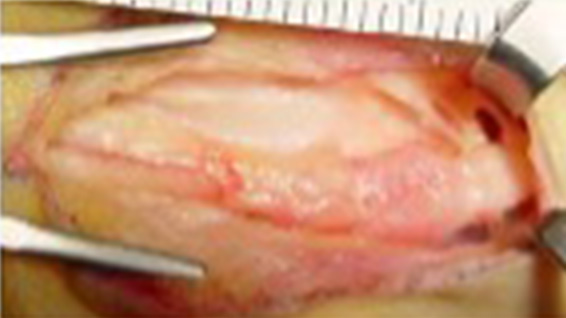 Photo courtesy of Peter Evans, MD, PhD
Photo courtesy of Peter Evans, MD, PhD
staged and recurrent procedures
In one study of patients with neurostenalgia following carpal tunnel decompression, nerve wrapping was associated with a significant reduction in visual analogue pain scores and improvement in patient satisfaction and symptom resolution (n=12). Patient-reported outcome measures demonstrated a significant reduction in hand disability.5
 Photo courtesy of Peter Evans, MD, PhD
Photo courtesy of Peter Evans, MD, PhD
other procedure types
Nerve protection can provide an ideal solution across surgical categories including decompressions, other trauma, head and neck, and iatrogenic injuries.
When there is trauma to structures adjacent to nerves, this not only hints at the force and mechanism of the injury’s origin but is highly indicative of the likelihood that nerves were involved. When surrounding structures such as ligaments and tendons are torn or transected, it is likely that the adjacent nerve is damaged as well.1
This common correlation highlights the importance of considering the pattern of injury when evaluating for possible nerve involvement.
provide a barrier to inflammatory cells and avoid soft tissue attachment
Adding a barrier between the non-transected nerve and the surrounding soft tissue gives the nerve a better chance at recovery by minimizing the possibility of soft tissue attachments, inflammatory macrophage invasion, and intraneural collagen deposition.
Minimizing soft-tissue attachment is essential because a nerve requires a healthy surrounding tissue bed to allow free nerve gliding.8
the right biomaterial for the right application
build a targeted barrier between nerves and soft-tissue attachment
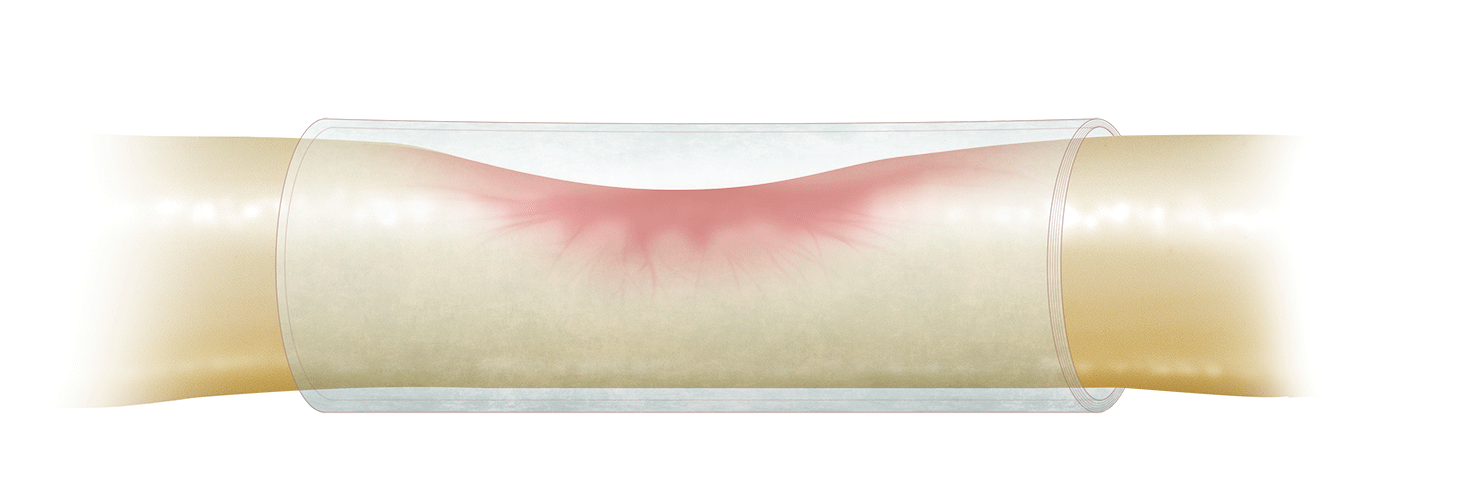
Scar tissue formation in the vicinity of a peripheral nerve can lead to damage, such as compression, ischemia, and impaired glide and tether, which can result in neurostenalgia.8 Neurostenalgia is a neuropathic pain that results from continuing irritation of an anatomically intact nerve by a noxious agent.
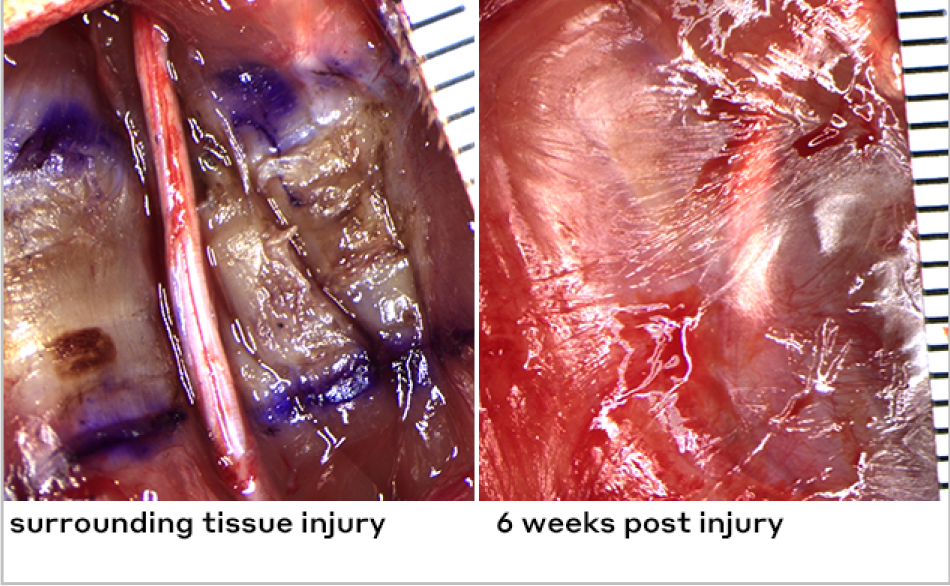
muscle injury: no wrap
Images of rat sciatic nerve, Axogen data on file.
muscle injury: with wrap
Images of rat sciatic nerve, Axogen data on file.
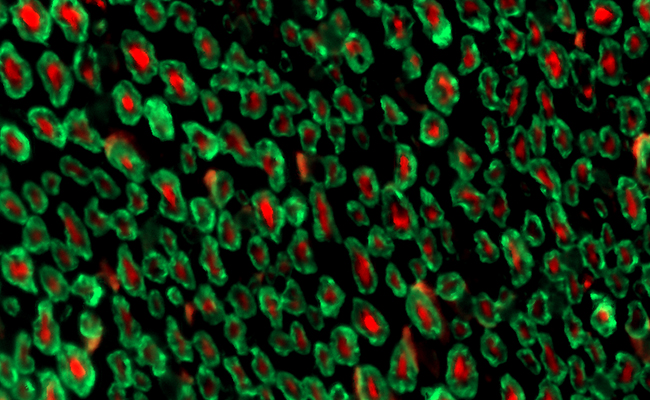
normal nerve fibers in a healthy tissue bed
axons: red | myelin: green
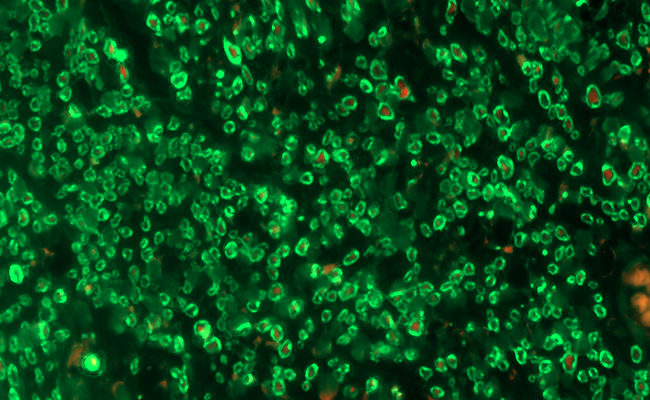
smaller nerve fibers (nerve injury) in an injured tissue bed
axons: red | myelin: green
With proper nerve protection, healthy, normal axons can remain undisturbed after injury to the surrounding tissue. As shown in the left image above from a preclinical study, the red staining represents the axons present in a healthy, normal nerve. Conversely, the image on the right represents a nerve that was sitting in an injured muscle bed and wasn’t protected. It shows little to no visible red staining because those axons have been damaged and aren’t there.2
When nerves are properly protected, less collagen buildup occurs. Collagen presence is often indicative of scarring.2
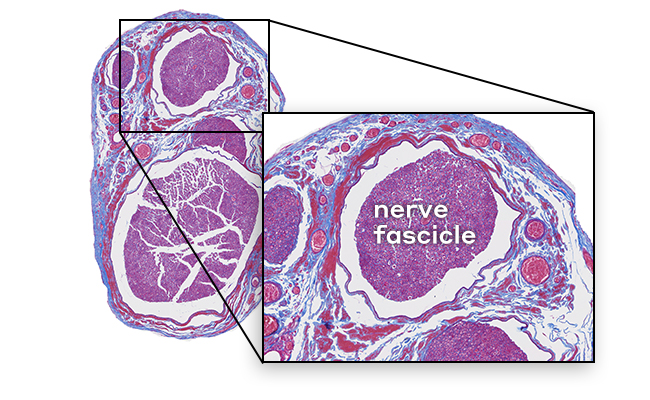
healthy epineurium and fascicles
cells: red | collagen: blue
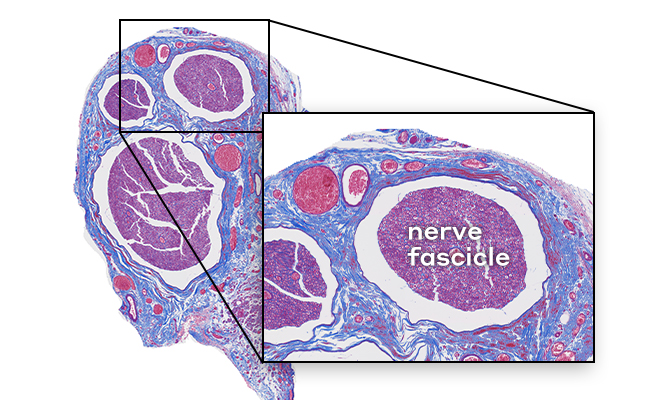
excess intraneural collagen (unprotected nerve in damaged tissue bed)
cells: red | collagen: blue
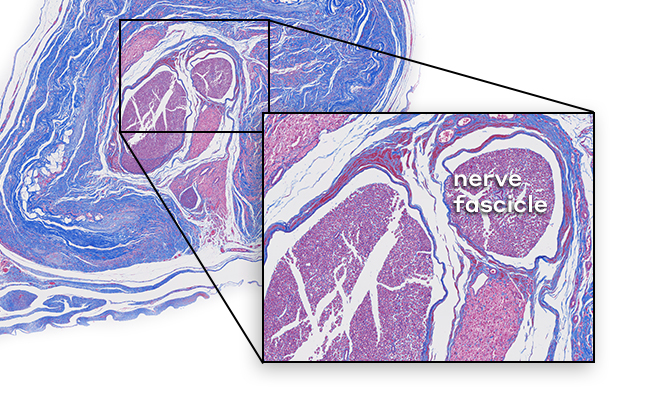
no excess intraneural collagen (nerve is protected from the damaged tissue bed by the collagen-based Axoguard HA+ Nerve Protector)
cells: red | collagen: blue
Protecting damaged nerves during the healing process is important for proper healing and consistent patient outcomes. Learn how our solutions help protect nerves from soft tissue attachments and mechanical irritation.

![]()
Remodeling extracellular matrix for long-term protection with a short-term gel coating for enhanced nerve gliding and minimization of soft tissue attachments.


Extracellular matrix that remodels to protect injured nerves and reinforce nerve reconstructions.


Avive+ Soft Tissue Matrix™ features a multi-layer amniotic tissue to protect acutely traumatized nerves and the surrounding area.
connect with a nerve rep
There’s only a short form between you and our nerve product team who can help you get more information about our nerve repair solutions.
educational events
Axogen offers a variety of events and opportunities for you to interact with experts and stay up to date on the most recent happenings in peripheral nerve surgery.
references
- Pereira DE, et al. Nerves in continuity following hand trauma: a descriptive report. Hand (N Y). 2023;18(1_suppl):126S-132S. doi:10.1177/15589447211064362
- Axogen data on file.
- Kokkalis ZT, et al. Assessment of processed porcine extracellular matrix as a protective barrier in a rabbit nerve wrap model. J Reconstr Microsurg. Jan 2011;27(1):19-28. doi:10.1055/s-0030-1267379
- Thomson SE, et al. Bioengineered nerve conduits and wraps for peripheral nerve repair of the upper limb. Cochrane Database Syst Rev. 2022;12(12):CD012574. doi:10.1002/14651858.CD012574.pub2
- Imran R, et al. Clinical outcomes following neurolysis and porcine collagen extracellular matrix wrapping of scarred nerves in revision carpal tunnel decompression. J Plast Reconstr Aesthet Surg. 2022;75(8):2802-2808. doi:10.1016/j.bjps.2022.04.010
- Voggenreiter G, et al. Immuno-inflammatory tissue reaction to stainless-steel and titanium plates used for internal fixation of long bones. Biomaterials. 2003;24(2):247-254. doi:10.1016/S0142-9612(02)00312-5
- Ricci FP, et al. Radial nerve injury associated with humeral shaft fracture: a retrospective study. Acta Ortop Bras. 2015;23(1):19-21. doi:10.1590/1413-78522015230100823
- Jordaan PW, et al. Management of the scarred nerve using porcine submucosa extracellular matrix nerve wraps. J Musculoskelet Surg Res. 2019;3:128-133. doi: 10.4103/jmsr.jmsr_69_18